Hyperparathyroidism: An In-Depth Exploration of Causes, Subtypes, Clinical Presentations, Diagnostic Approaches, and Treatment Modalities
Hyperparathyroidism represents a complex endocrine disorder characterized by dysregulation of parathyroid hormone (PTH) secretion, resulting in disturbances in calcium and phosphorus homeostasis. This comprehensive review aims to elucidate the multifaceted nature of hyperparathyroidism, encompassing its etiology, subtypes, clinical manifestations, diagnostic strategies, and therapeutic interventions.
Pathophysiology
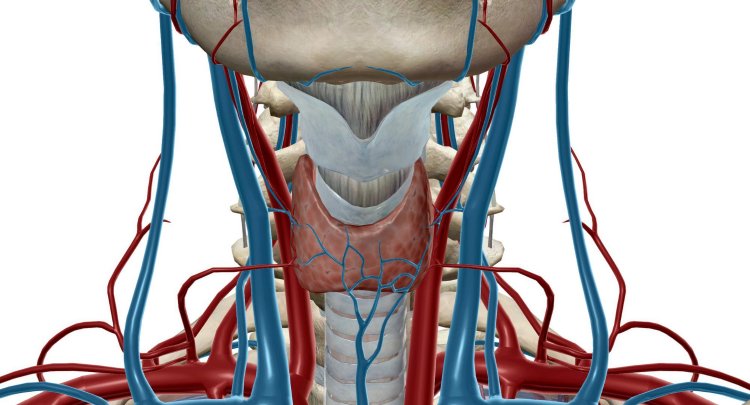
The pathophysiology of hyperparathyroidism revolves around aberrations in PTH synthesis, secretion, and action within the parathyroid glands and target organs. Primary hyperparathyroidism often arises from the development of solitary adenomas, multiple gland hyperplasia, or, rarely, parathyroid carcinoma. Secondary hyperparathyroidism, on the other hand, typically ensues as a compensatory response to systemic disorders, such as chronic kidney disease (CKD), vitamin D deficiency, or gastrointestinal malabsorption syndromes. Tertiary hyperparathyroidism represents a state of autonomous PTH secretion, often observed following prolonged secondary hyperparathyroidism.
Classification and Subtypes
1. Primary Hyperparathyroidism
Primary hyperparathyroidism constitutes the most prevalent form of the disorder and is primarily attributable to autonomous adenomatous or hyperplastic changes within the parathyroid glands. The clinical spectrum of primary hyperparathyroidism encompasses asymptomatic biochemical abnormalities, as well as overt manifestations of hypercalcemia, nephrolithiasis, osteoporosis, and neuropsychiatric disturbances.
2. Secondary Hyperparathyroidism
Secondary hyperparathyroidism arises secondary to chronic disturbances in calcium and phosphorus metabolism, commonly associated with renal insufficiency, vitamin D deficiency, or malabsorption syndromes. Persistent hypocalcemia and impaired vitamin D synthesis stimulate parathyroid gland hyperplasia and excessive PTH secretion, contributing to skeletal demineralization, renal calculi formation, and extraskeletal manifestations.
3. Tertiary Hyperparathyroidism
Tertiary hyperparathyroidism represents a state of persistent PTH hypersecretion following prolonged secondary hyperparathyroidism, typically observed in patients with end-stage renal disease (ESRD) who undergo renal transplantation or subtotal parathyroidectomy. Autonomous parathyroid adenomas or hyperplastic glands may continue to produce PTH independently of renal dysfunction, necessitating vigilant monitoring and potential resection.
Clinical Presentations and Complications
The clinical manifestations of hyperparathyroidism are diverse and may vary depending on the underlying subtype, disease duration, and individual patient factors. Musculoskeletal symptoms, including bone pain, fractures, and muscle weakness, are common features of hypercalcemia-induced osteoporosis and skeletal demineralization. Renal complications, such as nephrolithiasis, nephrocalcinosis, and renal insufficiency, may result from calcium precipitation within the renal parenchyma, impairing tubular function and promoting nephrotoxicity. Neuropsychiatric disturbances, cardiovascular abnormalities, and gastrointestinal symptoms further contribute to the clinical burden of hyperparathyroidism, necessitating comprehensive assessment and management.
Diagnostic Evaluation
The diagnostic evaluation of hyperparathyroidism encompasses a systematic approach to biochemical testing, imaging studies, and clinical assessment. Serum calcium and PTH levels serve as cornerstone laboratory parameters for diagnosing hypercalcemia and confirming inappropriate PTH secretion. Additional investigations, including renal function tests, urinary calcium excretion studies, dual-energy X-ray absorptiometry (DEXA) scans, and radiological imaging modalities (e.g., ultrasonography, sestamibi scintigraphy, CT, MRI), aid in localizing abnormal parathyroid tissue and assessing skeletal and renal involvement.
Treatment Strategies
The management of hyperparathyroidism necessitates a tailored approach based on the underlying etiology, disease severity, and presence of complications. Surgical intervention, in the form of parathyroidectomy, remains the definitive treatment for primary hyperparathyroidism and select cases of secondary and tertiary disease. Minimally invasive techniques, such as focused parathyroidectomy and intraoperative PTH monitoring, offer precise localization and maximal gland preservation, minimizing surgical morbidity. Pharmacological therapies, including calcimimetics, bisphosphonates, and vitamin D analogs, may be employed as adjunctive or alternative strategies to mitigate hypercalcemia, preserve bone density, and ameliorate symptomatic burden in nonsurgical candidates or refractory cases.
In conclusion, hyperparathyroidism represents a heterogeneous disorder characterized by dysregulated PTH secretion and perturbations in calcium and phosphorus metabolism. By elucidating the underlying pathophysiology, subtypes, clinical manifestations, diagnostic modalities, and therapeutic interventions associated with hyperparathyroidism, clinicians can facilitate early recognition, personalized management, and optimized outcomes for affected individuals.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
Hashtags
#Hyperparathyroidism #MedicalEducation #Healthcare #Endocrinology #BoneHealth
What's Your Reaction?





















