Beyond the Burn: Exploring the Depths of Peptic Ulcer Disease
Peptic ulcer disease (PUD) remains a significant gastrointestinal pathology, affecting millions of individuals worldwide. The interplay between various factors, including Helicobacter pylori infection, nonsteroidal anti-inflammatory drugs (NSAIDs), lifestyle choices, and genetic predisposition, contributes to the development of peptic ulcers. This article delves deeper into the mechanisms underlying PUD, its clinical presentation, diagnostic approaches, and contemporary management strategies.
Pathophysiology
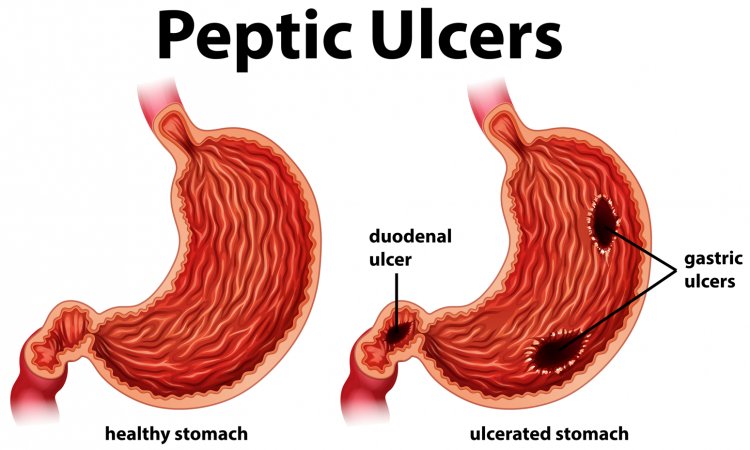
Peptic ulcers typically result from an imbalance between aggressive factors and mucosal defense mechanisms within the gastrointestinal tract. Aggressive factors include gastric acid secretion, pepsin activity, and H. pylori colonization, while protective mechanisms encompass mucosal integrity, bicarbonate secretion, and mucosal blood flow regulation. Disruption of this delicate equilibrium can lead to mucosal injury and ulcer formation.
Helicobacter pylori infection plays a central role in the pathogenesis of peptic ulcers by inducing chronic gastritis, impairing mucosal defenses, and promoting inflammation-mediated tissue damage. NSAIDs, particularly those inhibiting cyclooxygenase (COX) enzymes, compromise the integrity of the gastric mucosa by inhibiting prostaglandin synthesis, reducing mucosal blood flow, and increasing susceptibility to injury.
Clinical Presentation
The clinical presentation of peptic ulcer disease varies widely, ranging from asymptomatic to life-threatening complications. Common symptoms include epigastric pain, typically described as burning or gnawing, which may be exacerbated by fasting or relieved by food intake or antacids. Other manifestations encompass dyspepsia, bloating, belching, nausea, and vomiting.
Complications of PUD may include gastrointestinal bleeding, perforation, and gastric outlet obstruction. Gastrointestinal bleeding manifests as hematemesis (vomiting of blood), melena (black, tarry stools), or hematochezia (bright red blood in stools). Perforation presents with sudden, severe abdominal pain and signs of peritoneal irritation, necessitating urgent medical attention. Gastric outlet obstruction manifests as persistent vomiting, epigastric fullness, and weight loss.
Diagnostic Evaluation
The diagnosis of peptic ulcer disease involves a comprehensive evaluation encompassing clinical history, physical examination, and various diagnostic modalities. Endoscopic examination, typically esophagogastroduodenoscopy (EGD), remains the gold standard for identifying ulcerative lesions, assessing their size, location, and severity, and obtaining biopsy specimens for histological examination and H. pylori testing.
Additional diagnostic tests may include upper gastrointestinal series (barium swallow), which provides radiographic visualization of ulcerative lesions, and noninvasive tests for detecting H. pylori infection, such as serological assays, urea breath tests, and stool antigen tests.
Management Strategies
The management of peptic ulcer disease is multifaceted, aiming to alleviate symptoms, promote ulcer healing, eradicate H. pylori infection (if present), and prevent complications. Pharmacological interventions encompass proton pump inhibitors (PPIs), H2-receptor antagonists, mucosal protective agents, and antibiotics for H. pylori eradication.
Lifestyle modifications, including avoidance of NSAIDs, alcohol, and smoking, adoption of a healthy diet, stress reduction techniques, and weight management, play a crucial role in symptom management and ulcer prevention. Surgical intervention may be indicated in refractory cases, complicated ulcers, or in the presence of life-threatening complications.
Peptic ulcer disease remains a prevalent gastrointestinal disorder with significant morbidity and mortality. Understanding the intricate mechanisms underlying PUD, recognizing its diverse clinical presentations, and implementing appropriate diagnostic and therapeutic interventions are paramount for optimizing patient outcomes and reducing disease burden. Collaborative efforts between healthcare providers and patients are essential for the effective management and prevention of peptic ulcers.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
#Health #PepticUlcer #Gastroenterology #Healthcare #MedicalAdvice #PatientCare #Hygiene #GastricHealth
What's Your Reaction?





















