Type 1 Diabetes: Causes, Symptoms, Diagnosis, Treatment, and Complications
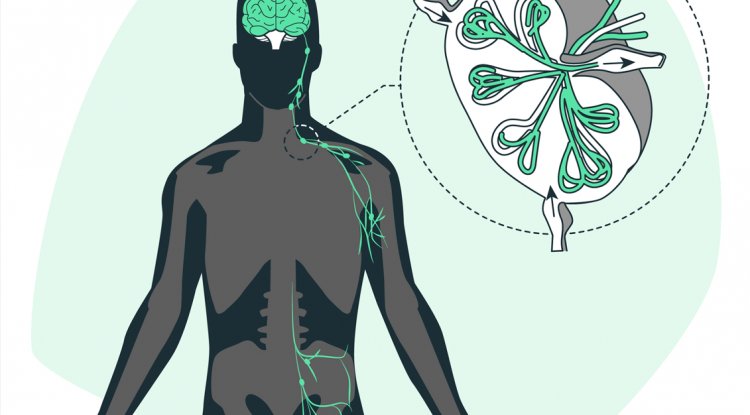
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas. This results in inadequate insulin production, leading to elevated levels of glucose in the bloodstream. Unlike type 2 diabetes, which is associated with insulin resistance, type 1 diabetes typically manifests early in life, although it can occur at any age.
Causes of Type 1 Diabetes
The precise cause of type 1 diabetes remains incompletely understood, but it is widely believed to involve a combination of genetic predisposition and environmental triggers. Certain genetic markers increase susceptibility to the condition, but environmental factors, such as viral infections or exposure to certain toxins, may also contribute to the autoimmune destruction of pancreatic beta cells.
Symptoms of Type 1 Diabetes
The symptoms of type 1 diabetes often develop rapidly and may include:
- Excessive Thirst (Polydipsia): High blood sugar levels prompt increased thirst as the body attempts to eliminate excess glucose through urine.
- Frequent Urination (Polyuria): Elevated blood glucose levels cause the kidneys to work harder to filter and absorb sugar, resulting in increased urination.
- Unexplained Weight Loss: Despite increased appetite, individuals with type 1 diabetes may experience weight loss due to the body's inability to utilize glucose for energy.
- Fatigue: Insufficient insulin prevents glucose from entering cells for energy production, leading to feelings of fatigue and weakness.
- Blurred Vision: High blood sugar levels can cause fluid to be pulled from the lenses of the eyes, resulting in blurred vision.
Diagnosis of Type 1 Diabetes
Diagnosis of type 1 diabetes typically involves blood tests to measure blood glucose levels, as well as tests to assess insulin levels and antibodies associated with the autoimmune destruction of pancreatic beta cells. These tests help differentiate type 1 diabetes from other forms of diabetes, such as type 2 diabetes or gestational diabetes.
Treatment of Type 1 Diabetes
Treatment for type 1 diabetes focuses on maintaining blood glucose levels within a target range to prevent complications. This typically involves a combination of the following:
- Insulin Therapy: Since individuals with type 1 diabetes produce little to no insulin, insulin therapy is essential for regulating blood sugar levels. This may involve multiple daily injections of insulin or the use of an insulin pump, which delivers insulin continuously throughout the day.
- Dietary Management: A balanced diet that includes carbohydrates, protein, and fat is crucial for managing blood sugar levels. Carbohydrate counting and meal planning can help individuals with type 1 diabetes better control their blood glucose levels.
- Regular Physical Activity: Exercise can improve insulin sensitivity and lower blood sugar levels. However, individuals with type 1 diabetes should monitor their blood sugar levels before, during, and after exercise to prevent hypoglycemia.
- Blood Sugar Monitoring: Regular monitoring of blood sugar levels is essential for adjusting insulin doses and making dietary and lifestyle modifications as needed. Continuous glucose monitoring systems provide real-time data on blood sugar levels, allowing for better management of the condition.
Complications of Type 1 Diabetes
Poorly controlled type 1 diabetes can lead to various complications over time, including:
- Cardiovascular Disease: High blood sugar levels can damage blood vessels and increase the risk of heart disease and stroke.
- Kidney Disease (Nephropathy): Diabetes is a leading cause of kidney failure, as high blood sugar levels can damage the kidneys over time.
- Nerve Damage (Neuropathy): Elevated blood sugar levels can cause nerve damage, leading to symptoms such as numbness, tingling, and pain, particularly in the hands and feet.
- Eye Damage (Retinopathy): Diabetes can damage the blood vessels in the retina, leading to vision problems and, in severe cases, blindness.
Conclusion
Type 1 diabetes is a chronic autoimmune condition characterized by the destruction of insulin-producing beta cells in the pancreas. While the exact cause remains unclear, both genetic predisposition and environmental factors are thought to contribute to its development. Early diagnosis and effective management are essential for preventing complications and maintaining overall health and well-being for individuals living with type 1 diabetes.
Through a comprehensive treatment approach that includes insulin therapy, dietary management, regular physical activity, and blood sugar monitoring, individuals with type 1 diabetes can lead fulfilling lives while effectively managing their condition. Ongoing research into the underlying mechanisms of type 1 diabetes and the development of new treatment options offer hope for improved outcomes and quality of life for those affected by this condition.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
#Type1Diabetes #DiabetesAwareness #HealthEducation #MedicalInformation #ChronicIllness #WellnessTips
What's Your Reaction?