The Bone Balancing Act: Managing Osteopenia for Optimal Health
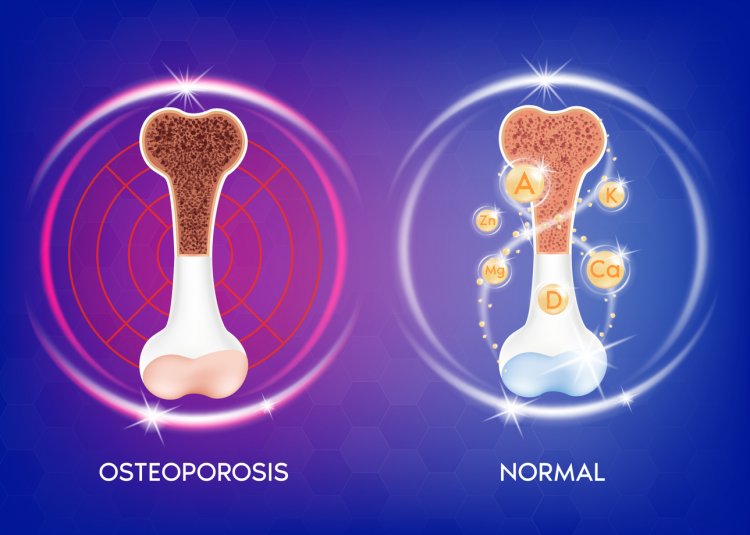
Osteopenia, a term often encountered in discussions about bone health, represents a condition characterized by lower bone mineral density (BMD) than normal but not to the extent of osteoporosis. It serves as a crucial intermediary stage in the spectrum of bone disorders, signaling a decline in bone strength and density that predisposes individuals to fractures and osteoporosis.
Defining Osteopenia:
Clinically, osteopenia is identified by BMD measurements falling between normal and osteoporotic ranges. This diagnostic categorization is established through dual-energy X-ray absorptiometry (DXA) scans, which calculate T-scores comparing an individual's BMD to that of a healthy young adult. A T-score between -1 and -2.5 standard deviations below the young adult mean indicates osteopenia.
Etiology of Osteopenia:
Age-Related Changes: Aging is a primary contributor to bone loss, with bone remodeling processes becoming less efficient over time. This age-related decline in bone density is more pronounced postmenopausally in women due to estrogen deficiency.
Hormonal Influences: Estrogen plays a vital role in maintaining bone density by inhibiting osteoclast-mediated bone resorption. Reduced estrogen levels postmenopausally accelerate bone loss, leading to osteopenia and osteoporosis.
Genetic Factors: Genetic predisposition contributes significantly to bone health, with familial patterns observed in osteoporosis and osteopenia risk.
Lifestyle Habits: Sedentary lifestyles, inadequate nutrition (particularly low calcium and vitamin D intake), smoking, excessive alcohol consumption, and prolonged use of corticosteroids or certain medications contribute to bone loss.
Medical Conditions: Various medical conditions, such as hyperthyroidism, celiac disease, rheumatoid arthritis, and hormonal disorders, can impact bone metabolism and increase the risk of osteopenia.
Recognizing Symptoms of Osteopenia:
Osteopenia often progresses asymptomatically until complications arise, typically in the form of fractures. However, individuals may experience:
- Gradual loss of height due to vertebral compression fractures.
- Back pain resulting from spinal fractures.
- Poor posture and spinal curvature (kyphosis).
Identifying Risk Factors for Osteopenia:
Understanding the risk factors associated with osteopenia aids in early detection and intervention:
- Gender and Age: Women, especially postmenopausal women, and older adults are at increased risk.
- Family History: A familial predisposition to osteoporosis or osteopenia elevates individual risk.
- Lifestyle Choices: Sedentary behavior, poor dietary habits, smoking, excessive alcohol consumption, and prolonged medication use contribute to bone loss.
- Medical Conditions: Chronic diseases affecting hormone levels or nutrient absorption may compromise bone health.
Diagnostic Approach to Osteopenia:
DXA scans remain the gold standard for diagnosing osteopenia, providing precise measurements of BMD and T-scores. Screening is recommended for postmenopausal women and men aged 50 and older, with periodic follow-ups based on individual risk factors.
Management and Treatment Strategies:
Addressing osteopenia involves multifaceted approaches aimed at preserving bone health and minimizing fracture risk:
- Lifestyle Modifications: Emphasize regular weight-bearing and muscle-strengthening exercises, adequate calcium (1000-1200 mg/day) and vitamin D (600-800 IU/day) intake, smoking cessation, and moderate alcohol consumption.
- Pharmacological Interventions: Depending on BMD levels and individual risk factors, healthcare providers may prescribe bisphosphonates, hormone replacement therapy (for postmenopausal women), or other medications to enhance bone density.
- Fall Prevention: Implement measures to reduce fall risk, such as modifying the home environment, using assistive devices, and addressing visual and balance impairments.
Preventive Strategies for Osteopenia:
Proactive measures to mitigate osteopenia progression and fracture risk include:
- Ensuring optimal nutritional intake, particularly calcium and vitamin D.
- Engaging in regular physical activity, including weight-bearing, resistance, and balance exercises.
- Undergoing regular bone density screenings as recommended by healthcare providers.
- Promoting awareness of bone health and fracture prevention in high-risk populations.
Exercise Recommendations for Osteopenia Management:
- Weight-bearing Exercises: Incorporate activities like walking, jogging, hiking, and stair climbing to stimulate bone formation and improve BMD.
- Resistance Training: Utilize resistance bands, free weights, or weight machines to strengthen muscles and bones, enhancing overall bone health.
- Balance and Flexibility Exercises: Practice yoga, tai chi, or Pilates to enhance balance, flexibility, and posture, reducing the risk of falls and fractures.
In conclusion, Osteopenia, though often overlooked in discussions about bone health, warrants attention as a significant precursor to osteoporosis and fractures. By comprehensively understanding the etiology, symptoms, diagnostic approaches, treatment modalities, preventive strategies, and exercise recommendations associated with osteopenia, individuals and healthcare providers can collaboratively work towards preserving bone health and minimizing the burden of osteoporotic fractures.
#Leukemia #AML #CML #ALL #CLL #Genetics #Environment #Hematology #Immunology #Symptoms #Diagnosis #Treatment #Prognosis #Survivorship #Research #Healthcare #CancerAwareness
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
What's Your Reaction?





















