Gut Check: A Comprehensive Guide to Inflammatory Bowel Disease
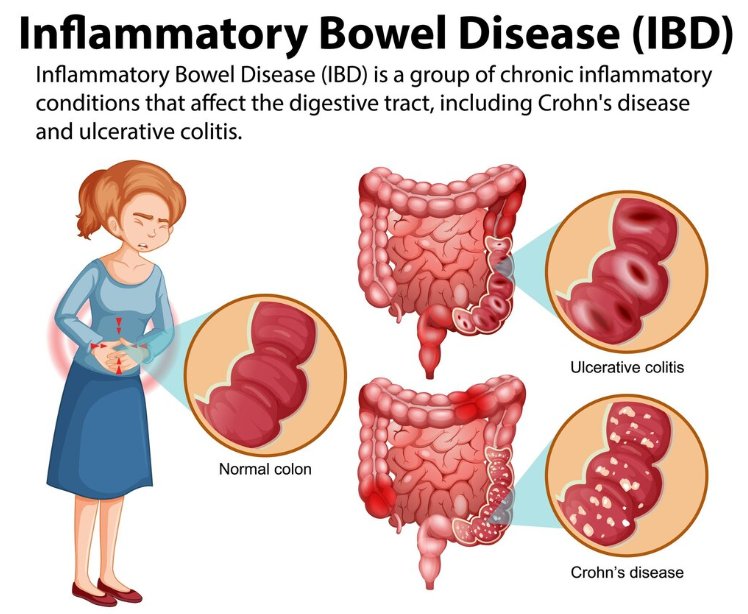
Inflammatory Bowel Disease (IBD) is an umbrella term used to describe disorders involving chronic inflammation of the digestive tract. The two main types of IBD are Crohn's disease and ulcerative colitis. Both conditions are characterized by periods of active disease (flare-ups) and periods of remission. IBD can significantly impact a person's quality of life, affecting physical, emotional, and social well-being.
Types of IBD
Crohn's Disease
Affected Areas: Crohn's disease can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. However, it most commonly impacts the end of the small intestine (the ileum) and the beginning of the colon.
Pattern of Inflammation: The inflammation in Crohn's disease can occur in patches and affect multiple layers of the bowel walls. This leads to deep ulcers, fistulas, and strictures.
Symptoms: Common symptoms include persistent diarrhea, abdominal pain and cramping, weight loss, fatigue, fever, and reduced appetite. Extra-intestinal manifestations can include arthritis, skin rashes, and eye inflammation.
Ulcerative Colitis
Affected Areas: Ulcerative colitis is restricted to the colon and rectum. The inflammation typically begins in the rectum and extends proximally in a continuous manner.
Pattern of Inflammation: Inflammation is limited to the mucosal layer of the colon, leading to the formation of ulcers.
Symptoms: Symptoms often include abdominal pain, frequent and urgent bowel movements, diarrhea mixed with blood or pus, rectal pain, rectal bleeding, weight loss, and fatigue. Patients may also experience systemic symptoms such as fever and anemia.
Causes and Risk Factors
Genetics: A significant genetic component is associated with IBD. Having a first-degree relative with IBD increases the risk of developing the condition. Specific genetic mutations, such as those in the NOD2 gene, have been linked to a higher susceptibility to Crohn's disease.
Immune System Dysfunction: An abnormal immune response is thought to play a crucial role in IBD. The immune system mistakenly attacks the cells of the intestines, causing chronic inflammation.
Environmental Factors: Various environmental triggers, including diet, smoking, use of NSAIDs, and certain infections, may contribute to the onset and exacerbation of IBD.
Age and Ethnicity: IBD can occur at any age but is commonly diagnosed in individuals between the ages of 15 and 35. Certain ethnic groups, particularly those of Ashkenazi Jewish descent, have a higher prevalence of IBD.
Diagnosis
The diagnosis of IBD involves a combination of clinical evaluation, laboratory tests, imaging studies, and endoscopic procedures:
Clinical Evaluation: A thorough medical history and physical examination are essential. Symptoms such as chronic diarrhea, abdominal pain, and weight loss warrant further investigation.
Blood Tests: These tests can reveal anemia, elevated inflammatory markers (like C-reactive protein and erythrocyte sedimentation rate), and signs of infection.
Stool Tests: These tests help rule out infections and detect blood or inflammatory markers in the stool.
Endoscopic Procedures: Colonoscopy and flexible sigmoidoscopy allow direct visualization of the colon and rectum. Biopsies taken during these procedures can confirm the diagnosis.
Imaging Studies: Cross-sectional imaging, such as CT enterography or MRI enterography, helps assess the extent and severity of the disease and detect complications like abscesses and fistulas.
Treatment
While there is no cure for IBD, several treatment options aim to reduce inflammation, manage symptoms, and achieve and maintain remission:
Medications:
- Aminosalicylates (5-ASAs): These anti-inflammatory drugs, such as mesalamine, are often used for mild to moderate ulcerative colitis.
- Corticosteroids: These are potent anti-inflammatory drugs used to induce remission in moderate to severe cases. Long-term use is limited due to potential side effects.
- Immunomodulators: Drugs like azathioprine, methotrexate, and 6-mercaptopurine suppress the immune system to reduce inflammation.
- Biologics: These are advanced therapies targeting specific components of the immune system. TNF inhibitors (e.g., infliximab, adalimumab), integrin inhibitors (e.g., vedolizumab), and interleukin inhibitors (e.g., ustekinumab) are commonly used biologics.
- Antibiotics: Used to treat or prevent infections, particularly in Crohn's disease with complications like abscesses.
- Pain Relievers and Supplements: Acetaminophen for pain management and supplements for nutritional deficiencies, such as iron, calcium, and vitamin D.
Diet and Nutrition: Tailored dietary plans can help manage symptoms. This may include low-residue diets to reduce bowel movements, avoiding trigger foods, and ensuring adequate nutrition through supplements if necessary.
Surgery: Surgery may be necessary for severe cases or complications. In Crohn's disease, this may involve resecting diseased segments of the intestine. For ulcerative colitis, a colectomy (removal of the colon) can be curative.
Complications
IBD can lead to several complications if not adequately managed:
Bowel Obstruction: Chronic inflammation can cause scarring and narrowing of the intestines, leading to obstruction.
Fistulas: Abnormal connections between different parts of the bowel or between the bowel and other organs can develop, particularly in Crohn's disease.
Strictures: Severe narrowing of the bowel can result from chronic inflammation and scarring.
Perforation: Severe inflammation can cause a hole in the bowel wall, leading to peritonitis.
Nutritional Deficiencies: Poor absorption of nutrients can lead to deficiencies in vitamins and minerals, contributing to osteoporosis, anemia, and other health issues.
Increased Cancer Risk: Long-standing IBD, particularly ulcerative colitis, increases the risk of colorectal cancer.
Extra-intestinal Manifestations: IBD can cause inflammation in other parts of the body, including the skin, eyes, joints, and liver.
Living with IBD
Managing IBD requires a holistic approach, including medical treatment, lifestyle modifications, and psychological support:
Regular Medical Care: Frequent monitoring and follow-up with a gastroenterologist are essential to manage the disease and adjust treatments as necessary.
Diet and Nutrition: Working with a dietitian can help tailor a diet that minimizes symptoms and ensures adequate nutrition.
Stress Management: Techniques such as mindfulness, meditation, yoga, and counseling can help manage stress, which can exacerbate symptoms.
Exercise: Regular physical activity can improve overall health, reduce stress, and alleviate some symptoms.
Support Networks: Joining support groups and connecting with others who have IBD can provide emotional support and practical advice.
In conclusion, Inflammatory Bowel Disease is a chronic and complex condition requiring comprehensive management. Early diagnosis, personalized treatment plans, and a multidisciplinary approach are crucial in improving the quality of life for individuals with IBD. Ongoing research continues to improve our understanding of the disease and develop more effective treatments. With proper medical care and lifestyle adjustments, many people with IBD can lead fulfilling lives despite the challenges posed by the disease.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
#IBD #CrohnsDisease #UlcerativeColitis #Health #Wellness #ChronicIllness #GutHealth #AutoimmuneDisease #Inflammation #MedicalAdvice #Nutrition #SupportNetworks
What's Your Reaction?





















