From Pain to Power: Transformative Insights into Hysterectomy
Hysterectomy, the surgical removal of the uterus, is one of the most frequently performed gynecological surgeries worldwide. This procedure can be life-changing, affecting a woman's reproductive abilities and hormonal balance. Understanding the different types of hysterectomies, the conditions that necessitate this surgery, the various surgical techniques, and the recovery process is essential for patients and healthcare providers alike. This comprehensive overview will delve into these aspects in detail, providing a thorough understanding of hysterectomy.
Types of Hysterectomy
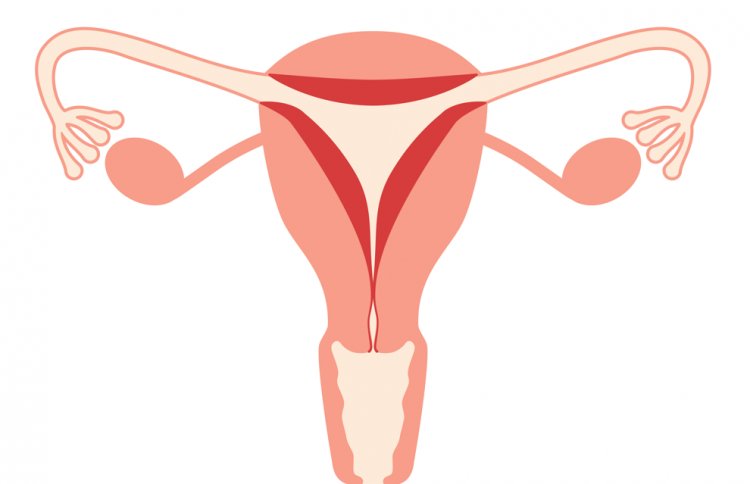
What is a Hysterectomy?
A hysterectomy is a surgical procedure to remove the uterus, the muscular organ in a woman's reproductive system where a fetus develops during pregnancy. This document provides information on the different types of hysterectomy, reasons why a hysterectomy might be recommended, surgical approaches, recovery, and potential complications. It is important to note that this information is for educational purposes only and should not be substituted for professional medical advice. Always consult with a healthcare provider for proper diagnosis and treatment of any medical condition.
Types of Hysterectomy (Based on Extent of Removal)
-
Total Hysterectomy: This is the most common type of hysterectomy. During this procedure, the surgeon removes the entire uterus, including the cervix, which is the lower, narrow end of the uterus that connects to the vagina.
-
Partial (Subtotal) Hysterectomy (Supracervical Hysterectomy): In this procedure, only the upper part of the uterus is removed, leaving the cervix intact. This option may be suitable for some women depending on the underlying medical condition.
-
Radical Hysterectomy: This is a more extensive surgery typically performed for cancer treatment. The surgeon removes the uterus, cervix, upper part of the vagina, and surrounding tissues, which may include pelvic lymph nodes.
Indications for Hysterectomy
Hysterectomy may be recommended for various reasons, often after other treatments have been unsuccessful. Here are some common reasons a hysterectomy might be considered:
-
Uterine Fibroids: These are non-cancerous growths in the uterus that can cause significant symptoms, including heavy menstrual bleeding, pelvic pain, and pressure on the bladder or bowel.
-
Endometriosis: This condition occurs when tissue similar to the uterine lining grows outside the uterus, causing chronic pain and infertility.
-
Uterine Prolapse: This condition happens when the uterus descends into the vaginal canal due to weakened pelvic muscles and ligaments.
-
Chronic Pelvic Pain: Persistent pelvic pain that does not respond to other treatments may necessitate a hysterectomy.
-
Cancer: Hysterectomy is a common treatment for cancers of the uterus, cervix, ovaries, or endometrium.
-
Abnormal Uterine Bleeding: Severe and unmanageable uterine bleeding, unresponsive to other treatments, may lead to hysterectomy.
Surgical Approaches
There are several ways to perform a hysterectomy, each with its own advantages and limitations. The best surgical approach for you will depend on various factors, such as the underlying medical condition, the size and location of the uterus, and your overall health. It is important to discuss these options with your healthcare provider to determine the most suitable approach for your individual situation.
-
Abdominal Hysterectomy: This approach involves an incision in the lower abdomen to access and remove the uterus. It is often used when a large uterus or cancer is involved. The recovery period for an abdominal hysterectomy is typically longer compared to other methods.
-
Vaginal Hysterectomy: The uterus is removed through an incision in the vagina during a vaginal hysterectomy. This method avoids external scarring and generally has a shorter recovery period compared to an abdominal hysterectomy.
-
Laparoscopic Hysterectomy: This is a minimally invasive technique that uses small incisions in the abdomen and a laparoscope (a small camera) to guide the surgery. There are different variations of laparoscopic hysterectomy, including:
-
Laparoscopic-Assisted Vaginal Hysterectomy (LAVH): This combines laparoscopic and vaginal approaches, allowing for better visualization and access during surgery.
-
Robotic-Assisted Laparoscopic Hysterectomy: This technique uses robotic technology to enhance precision and control during surgery.
-
Recovery and Aftercare
The recovery process after a hysterectomy varies depending on the surgical approach used. Here's a general overview of recovery times for different procedures:
-
Abdominal Hysterectomy: Recovery can take 4-6 weeks, with a hospital stay of 2-4 days. Patients need to avoid strenuous activities and heavy lifting during the recovery period.
-
Vaginal and Laparoscopic Hysterectomies: These methods generally offer a quicker recovery, around 2-4 weeks, with shorter hospital stays of 1-2 days. Patients can usually return to normal activities sooner compared to an abdominal hysterectomy.
Following surgery, proper care is crucial for optimal healing and minimizing complications. This may include pain management, wound care, and gradual resumption of daily activities as instructed by your healthcare provider. Regular follow-up visits are essential to monitor recovery and address any issues that may arise.
Potential Complications
While hysterectomy is generally safe, it's not without potential risks and complications. It's important to discuss these with your healthcare provider before surgery. Here are some key concerns:
- Injury to surrounding organs: The bladder, intestines, or blood vessels may be accidentally damaged during surgery.
- Blood clots: There's a risk of developing deep vein thrombosis (DVT) or pulmonary embolism, especially after abdominal surgery.
- Hormonal changes (if ovaries removed): Removing the ovaries (oophorectomy) can trigger sudden menopause, affecting hormone levels and causing symptoms like hot flashes and bone loss.
- Emotional impact: Some women may experience feelings of loss or depression, particularly if the hysterectomy affects their sense of femininity or fertility.
In conclusion, Hysterectomy is a significant surgical intervention with various types tailored to different medical conditions. It is essential for patients to understand the reasons for the surgery, the surgical options available, and the recovery process. By comprehending the potential risks and benefits, patients can make informed decisions in collaboration with their healthcare providers. Proper preoperative and postoperative care is crucial to minimize complications and enhance recovery, ensuring the best possible outcomes for those undergoing hysterectomy.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
#hysterectomy #womenshealth #surgery #recovery #fibroids #endometriosis #uterineprolapse #chronicpelvicpain #cancer #bleeding #laparoscopy #abdomen #vagina #laparoscopicassistedvaginalhysterectomy #roboticassistedlaparoscopic #aftercare #complications
What's Your Reaction?