From Diagnosis to Treatment: The Journey of Beta Thalassemia Patients
Beta thalassemia is a hereditary blood disorder marked by reduced production of hemoglobin, the essential protein in red blood cells responsible for oxygen transport throughout the body. This condition arises from mutations in the HBB gene, which encodes the beta-globin subunit of hemoglobin. Beta thalassemia is most commonly observed in Mediterranean countries, the Middle East, Central Asia, India, and Southeast Asia. This article delves into the intricate details of the causes, symptoms, diagnosis, and treatment options for beta thalassemia.
Causes
The fundamental cause of beta thalassemia is mutations in the HBB gene on chromosome 11. These mutations result in the reduced or absent production of beta-globin chains, creating an imbalance between alpha and beta chains in hemoglobin. This imbalance leads to the formation of abnormal hemoglobin, which precipitates ineffective erythropoiesis (production of red blood cells) and hemolysis (destruction of red blood cells).
Beta thalassemia is inherited in an autosomal recessive pattern. This means an individual must inherit two defective genes, one from each parent, to exhibit the severe symptoms of the disease. Individuals with only one defective gene are carriers, often asymptomatic or presenting with mild anemia, and are referred to as having beta thalassemia minor or trait.
Pathophysiology
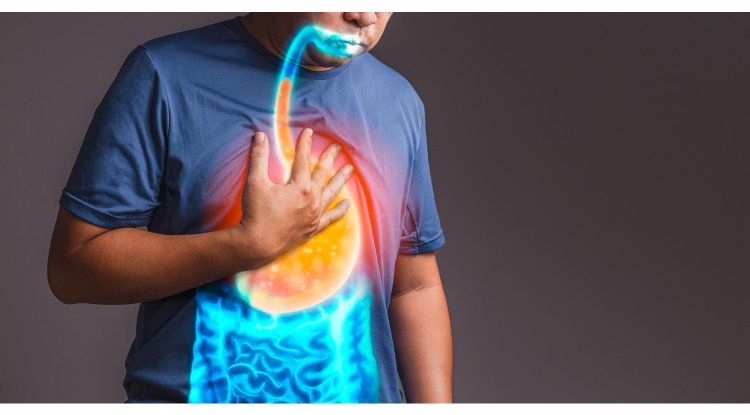
The pathophysiology of beta thalassemia revolves around the defective synthesis of beta-globin chains. This defect disrupts the formation of normal hemoglobin (HbA), leading to an excess of unpaired alpha-globin chains. These unpaired chains precipitate within red blood cells, causing oxidative damage and premature destruction of the cells in the bone marrow (ineffective erythropoiesis) and in the spleen (hemolysis). The resulting chronic anemia triggers compensatory mechanisms, including bone marrow expansion and increased erythropoietin production, leading to bone deformities and extramedullary hematopoiesis.
Clinical Manifestations
The clinical manifestations of beta thalassemia vary depending on the specific mutations and the amount of functional beta-globin produced. The three main forms of beta thalassemia are:
Beta Thalassemia Major (Cooley's Anemia)
Onset: Symptoms typically appear within the first two years of life.
Symptoms: Severe anemia, jaundice, growth retardation, skeletal deformities (especially facial bones), hepatosplenomegaly (enlarged liver and spleen), and delayed puberty.
Complications: Without regular blood transfusions, children with beta thalassemia major can suffer from severe complications, including heart failure, endocrine dysfunctions, and increased susceptibility to infections.
Beta Thalassemia Intermedia
Onset: Symptoms manifest later in childhood or adolescence.
Symptoms: Moderate anemia, growth delays, bone deformities, and splenomegaly. Symptoms are less severe compared to beta thalassemia major.
Management: Patients may require occasional blood transfusions and iron chelation therapy but generally have a milder clinical course.
Beta Thalassemia Minor (Trait)
Symptoms: Individuals are typically asymptomatic or exhibit mild anemia that may go unnoticed. They usually lead normal lives without significant health issues.
Diagnosis: Often diagnosed incidentally during routine blood tests or genetic screening.
Diagnosis
Diagnosing beta thalassemia involves several diagnostic tests and evaluations:
Complete Blood Count (CBC)
- Reveals microcytic hypochromic anemia (small, pale red blood cells) and reduced mean corpuscular volume (MCV).
- Increased red blood cell count with a low hemoglobin level.
Hemoglobin Electrophoresis
- Measures different types of hemoglobin in the blood.
- In beta thalassemia, abnormal levels of hemoglobin A2 and hemoglobin F are typically found.
Genetic Testing
- DNA analysis can identify specific mutations in the HBB gene.
- Confirms the diagnosis and helps determine the type of beta thalassemia.
Prenatal Testing
- For couples at risk of having a child with beta thalassemia major, prenatal testing through chorionic villus sampling (CVS) or amniocentesis can detect the condition in the fetus.
- Preimplantation genetic diagnosis (PGD) can be used in conjunction with in vitro fertilization (IVF) to prevent the birth of affected children.
Treatment
The treatment of beta thalassemia depends on the severity of the disease and aims to manage symptoms and prevent complications:
Regular Blood Transfusions
- Patients with beta thalassemia major require regular blood transfusions, typically every 2-4 weeks, to maintain hemoglobin levels and alleviate anemia symptoms.
- Transfusions help suppress ineffective erythropoiesis and reduce extramedullary hematopoiesis.
Iron Chelation Therapy
- Repeated blood transfusions lead to iron overload, which can damage organs such as the heart, liver, and endocrine glands.
- Iron chelation therapy (e.g., deferoxamine, deferasirox, deferiprone) helps remove excess iron from the body and prevent complications of iron overload.
Folic Acid Supplements
- Folic acid supports the production of red blood cells and is often prescribed to patients with beta thalassemia.
Bone Marrow Transplant (BMT)
- Currently, the only potential cure for beta thalassemia.
- Involves replacing the diseased bone marrow with healthy marrow from a compatible donor.
- BMT carries significant risks, including graft-versus-host disease (GVHD) and requires a suitable donor, often a matched sibling.
Gene Therapy
- Emerging treatments involve correcting the genetic defect in hematopoietic stem cells.
- Clinical trials are ongoing, and while promising, these treatments are still under investigation.
Splenectomy
- Surgical removal of the spleen may be considered in patients with significant splenomegaly or hypersplenism (overactive spleen).
- Reduces the need for blood transfusions but increases the risk of infections.
Beta thalassemia is a complex genetic disorder with a wide range of clinical manifestations. Advances in medical research and treatment have significantly improved the quality of life and life expectancy for patients with beta thalassemia major. Early diagnosis, regular monitoring, and appropriate therapeutic interventions are crucial in managing the disease effectively. Continued research into gene therapy and other innovative treatments offers hope for a future where beta thalassemia can be effectively cured or managed with minimal complications. Awareness and genetic counseling are essential for at-risk populations to prevent the transmission of beta thalassemia and reduce its global burden.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
#Hashtags: #BetaThalassemia #GeneticDisorders #Health #MedicalResearch #BloodDisorders
What's Your Reaction?