Battling Bacteremia: Strategies for Detecting and Defeating Bloodstream Invaders
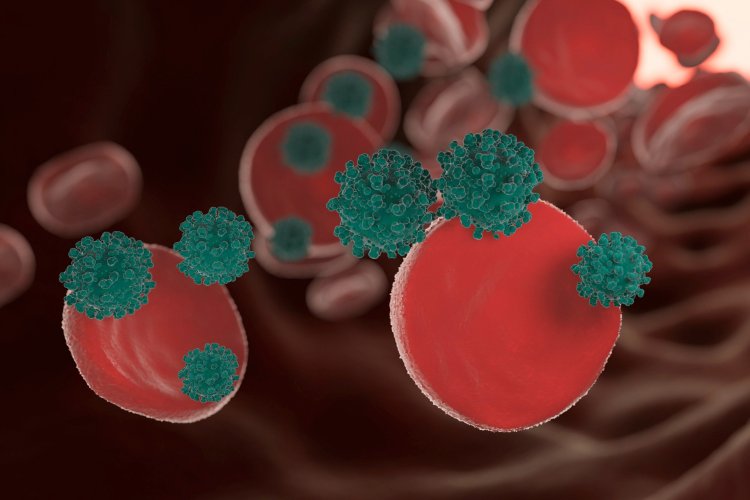
Bacteremia, a condition characterized by the presence of bacteria in the bloodstream, poses a significant threat to human health. While the bloodstream is typically considered sterile, the introduction of bacteria into this environment can have serious consequences. This article delves into the intricate aspects of bacteremia, exploring its etiology, clinical manifestations, diagnostic approaches, treatment modalities, and preventive strategies.
Etiology
Bacteremia can arise from a myriad of sources, often stemming from breaches in the body's natural defenses. The following are common etiological factors:
- Infectious Foci: Localized infections, ranging from respiratory tract infections like pneumonia to genitourinary infections such as pyelonephritis, can serve as primary reservoirs for bacterial dissemination into the bloodstream.
- Invasive Medical Procedures: Surgical interventions, indwelling catheters, and invasive medical devices create portals of entry for bacteria, facilitating their entry into the bloodstream.
- Trauma and Injury: Skin abrasions, wounds, and traumatic injuries compromise the skin's integrity, enabling bacterial infiltration into the bloodstream.
- Underlying Health Conditions: Individuals with compromised immune systems, such as those suffering from HIV/AIDS or undergoing immunosuppressive therapy, are predisposed to bacteremia.
Clinical Manifestations
The clinical presentation of bacteremia can vary widely, influenced by factors such as the virulence of the infecting organism and the host's immune status. Common manifestations include:
- Systemic Symptoms: Fever, chills, and malaise are hallmark features of bacteremia, reflecting the body's systemic inflammatory response.
- Hemodynamic Instability: Severe cases may manifest as hypotension (septic shock), tachycardia, and altered mental status, indicative of systemic compromise.
- Localized Symptoms: Depending on the source of infection, patients may exhibit signs of localized inflammation, such as erythema, warmth, and tenderness at the site of infection.
Diagnostic Approaches
The diagnosis of bacteremia hinges on a comprehensive evaluation encompassing clinical, laboratory, and imaging modalities:
- Blood Cultures: Collection of blood specimens for culture and sensitivity testing remains the cornerstone of bacteremia diagnosis, facilitating the identification of causative organisms and their antibiotic susceptibilities.
- Laboratory Investigations: Ancillary laboratory tests, including complete blood count (CBC), inflammatory markers (e.g., C-reactive protein), and coagulation studies, aid in assessing the severity of infection and its systemic impact.
- Imaging Studies: Radiographic imaging, such as chest X-rays, abdominal ultrasound, or computed tomography (CT) scans, may be warranted to localize the source of infection and assess for complications like abscess formation.
Treatment Modalities
Effective management of bacteremia entails a multipronged approach aimed at eradicating the underlying infection and mitigating systemic sequelae:
- Empirical Antibiotic Therapy: Prompt initiation of broad-spectrum antibiotics is imperative pending culture results, with subsequent tailoring of therapy based on microbiological data.
- Source Control Measures: Surgical debridement, abscess drainage, or removal of infected devices are integral components of treatment aimed at eliminating the source of bacteremia.
- Supportive Care: Hemodynamic stabilization, fluid resuscitation, and vasopressor support may be necessary in cases of septic shock to maintain end-organ perfusion and prevent multiorgan dysfunction.
Preventive Strategies
Prevention of bacteremia revolves around proactive measures targeting both individual and healthcare-associated risk factors:
- Hand Hygiene: Rigorous adherence to hand hygiene protocols, including handwashing with soap and water or alcohol-based hand sanitizers, is paramount in reducing bacterial transmission.
- Aseptic Techniques: Healthcare providers must adhere to strict aseptic practices during invasive procedures, catheter insertions, and wound care to minimize the risk of iatrogenic bacteremia.
- Immunization: Vaccination against specific pathogens, such as Streptococcus pneumoniae and Neisseria meningitidis, confers protection against infections that can lead to bacteremia.
- Chronic Disease Management: Optimal control of underlying medical conditions, including diabetes mellitus and chronic kidney disease, is pivotal in bolstering host defenses against bacterial invasion.
Conclusion
Bacteremia represents a formidable clinical entity necessitating a nuanced approach to diagnosis, treatment, and prevention. By elucidating the intricate interplay between microbial virulence and host susceptibility, clinicians can adopt tailored strategies aimed at optimizing patient outcomes. Through continued research efforts and vigilant adherence to evidence-based practices, the medical community remains steadfast in its commitment to combatting the scourge of bacteremia and its associated complications.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered medical advice. If you have any health concerns or are experiencing symptoms, it is important to consult with a healthcare professional, such as a doctor or clinic, for proper diagnosis and treatment. Always seek the advice of your doctor or other qualified health provider with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay in seeking it because of something you have read in this article.
Hashtags
#Bacteremia #InfectiousDisease #HealthCare #MedicalEducation #PreventiveCare
What's Your Reaction?





















